After sharing about my recent trip to Davao City, I came across one of my older videos on Youtube –it was a short little video entitled “pre-residency 2021“.
It’s been twenty-one months since I started residency. Honestly: wild.
In this career-related blog post:
- Growing in my roots – Family Practice Center and Community Medicine
- Finding places to bloom – Toxicology Subspecialty, Lifestyle Medicine, Medical Sign Language and Family Health Liaison
- Thriving with love (it’s a continuous process)
Roots.
We don’t have our own admitting ward (naturally), and we don’t have only one community clinic to rotate in. The “Family Practice Center” outpatient clinic is the homebase of FCM residents. At least 6 months in first year, 4 months in second year, and 2 months plus some change in third year is spent in this clinic.

.
One of the core competencies and training activities of our department is systems management. I’m sure it’s not unique to our program, but just getting to think and change processes outside my individual sphere of influence is one of the things I appreciate the most. I didn’t even know that was a thing when I was a pre-resident. (Though there are days when our exercises tend to be more theoretical than applied…)
Our systems-thinking crosses everything, from our outpatient clinic to our interactions with other departments in the ED, and to our rotations outside the hospital. We spend 2 months in first year, 1 month in second year, and a total of 4 months in third year rotating in the rural then urban community.
We try not to just treat individual patients. In fact, you’d probably fail community rotation without an attempt to at least contribute to the hospital-community partnership.

I had the fortune to be assigned to the same local health center as last year, so I saw how big a difference several months makes. Because of the Universal Health Care Act, and the local changes being made by the Manila Health Department, Manila health centers have undergone a major overhaul. Mostly for the good —more accessible free laboratories and medications, increased accessibility for PWD, higher patient subscription. But naturally there remain challenges and limitations, mainly in the form of the still-nascent electronic medical record and the manpower shortages.
Last year, I had the pleasure to start a competency-building health lecture and workshop series with our urban community partner in Baseco. This month our activities were mostly centered around nutrition, as well as organization development.
.
Read here: from womb to tomb (and the before, during and after of compassionate care)

.
In between the outpatient clinic and our formal partners with the Manila Health Department/CDP, there were also other moments to exercise and celebrate our patient-centered, family-focused and community-oriented approach. I’ll probably run out of space if I try to name them all.
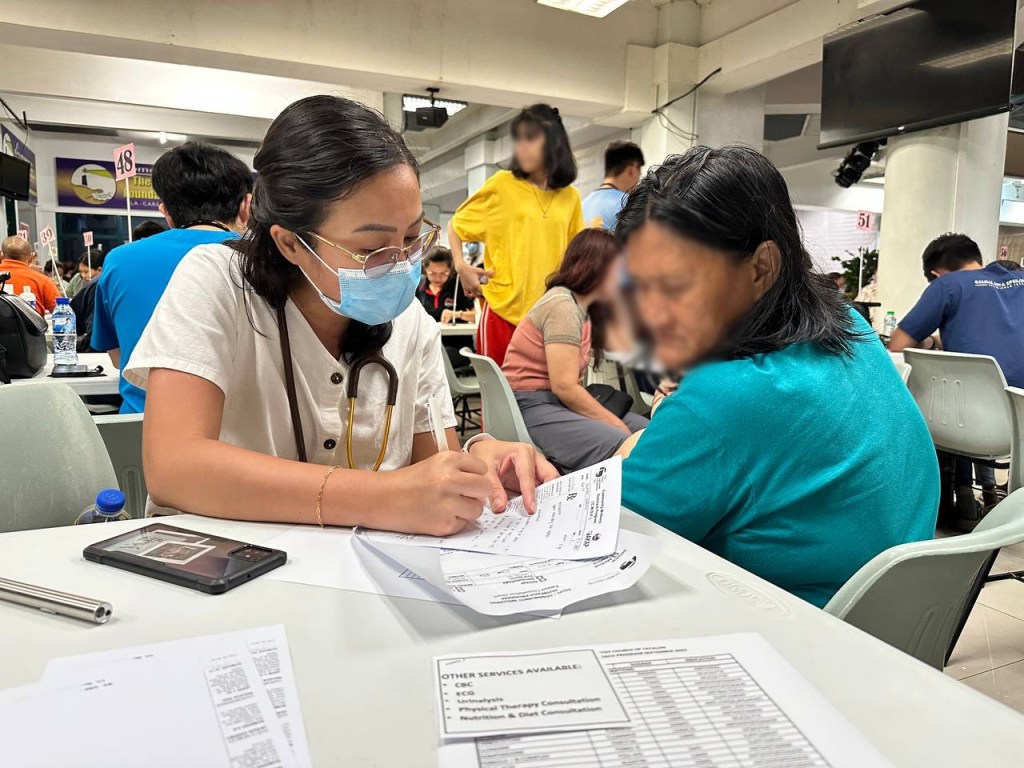
To our congressmen, legislators, executive officials: Can’t we just open our local health centers for two Saturdays a month (and correspondingly close them for two weekdays a month), with the appropriate overtime pay, just so indigent patients, workers with weekday jobs, and kids with school can benefit from truly accessible services? Instead of cramming everyone into one day like this, every six months?
Thank you.
.
Bloom.
Seeing outpatient consults day-in and day-out is mindnumbing if it stretches out for more than two months at a time. (Which was me, this last August and September. I am a little more than ready to take a break).
So it’s nice to have the chance to serve and learn elsewhere —to grow a little bit more while keeping the family-focused and community-oriented perspective firmly in hand.
I remember starting this year with the blurriest two months of my second-year life. General Medicine tested my grit and patience, and also probably the patience of my seniors who had to answer my burning clinical questions at odd hours of the night. In Toxicology, I fared a little better and life was a lot kinder. My only other non-FPC or clinical rotation was research.
Read Here: One must not imagine Sisyphus happy, and other thoughts while rotating in Internal Medicine
There’s a use case argument for family medicine practitioners as part of the inpatient team —referred to counsel patients and their loved ones, help in resource navigation or home care planning, support in decision-making, and more. There is already a similar role played by SHPM subspecialists, but not all those requiring family-level interventions are necessarily palliative or hospice patients. Thoughts for the future.
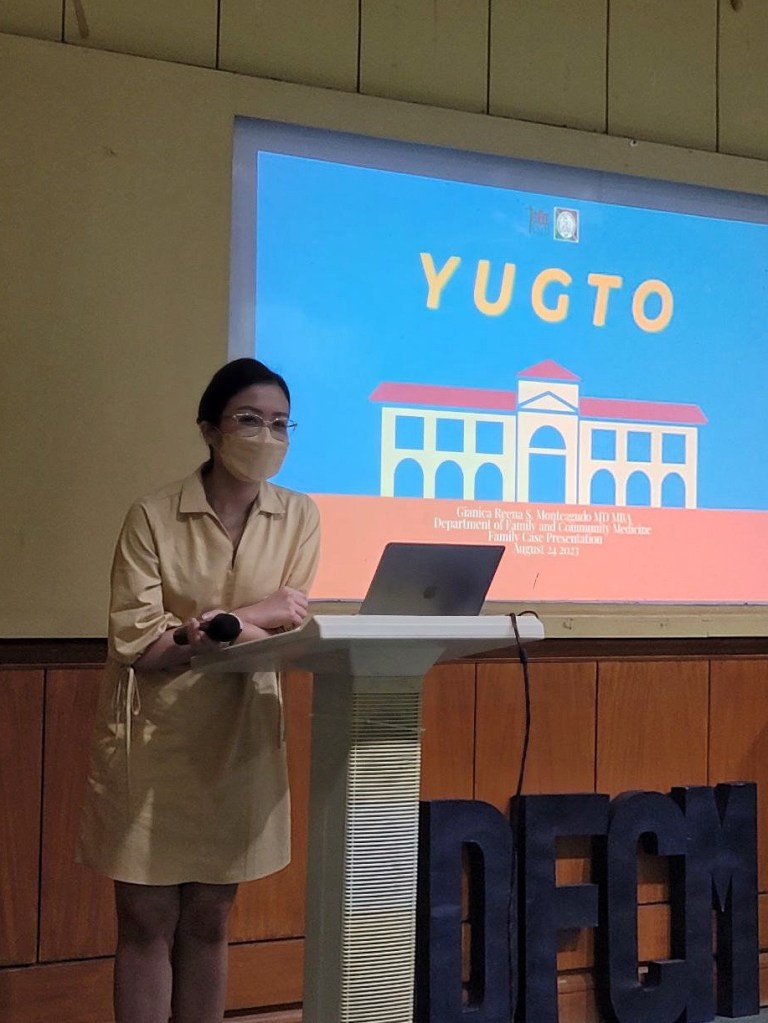
Featuring yet another neutral dress from STRAIGHTFORWARD.
.

Internists, pediatricians, and FCM specialists can train in PGH (and a few other tertiary hospitals like EAMC). The approach to toxicology remains holistic —because many of the cases are non-accidental, and require a delicate touch— but they also require a deep understanding of pharmacology. At this point, toxicology isn’t in my list of likely career tracks, but never rule out the anything.
But please, to our national government and DOH: can we please give our National Poison Management and Control Center actual budget for a (1) more equipment and personnel to actually handle the nationwide hotline, and (2) a functioning and automized electronic database for reporting of cases?
.

Tip I wish I heard before this day: wear all-black for duty. You never know when you’ll be mixing and administering activated charcoal.
.

.

It’s been around two to three months since. I’ve forgotten some things without the practice; I really need to rewatch the lessons, get started on finding a practice buddy, and enroll in the next class. Ultimately, I want to be a certified interpreter.
.
Read here: Baby Steps in Filipino Sign Language – Training with DeafEd Philippines

Decisions like that are rarely easy, but getting a glimpse of other possibilities can only help. A few weeks or so ago, our department conference invited the pioneer in Lifestyle Medicine, Dr. Palma, for a talk on its origins in the country, evidence-based practices, and advice on pursuing training. I’ve always felt strongly about wellness and holistic care. Maybe.
(If only I could get my elective on lifestyle medicine off the ground!)
.

Most times this includes family counselling for wellness or for families with chronic diseases, but sometimes this also includes coordination of care with multidisciplinary clinics. Just the other week I attended a MDC with Developmental Pediatrics, Adolescent Medicine, Psychiatry, and CAMP; in the context of youth with developmental disabilities (such as children with Autisim or Down Syndrome), continuity of care and care for the family, caregiver burnout screening, community resource navigation, and so on are just as important as the initial rehabilitation and care.
.
Aside from our participation in the Transition Clinic-Youth with Developmental Disabilities MDC, we are also part of the inpatient Ortho-Geriatric Fracture Liaison Service, the Osteoarthritis MDC, Smoking Cessation Clinic, W3E2 Talk Weight Management MDC, and some more still in development. While our partners in the team focus on the biomedical, we focus on the biopsychosocial, family, and socioeconomic environment.
Thrive.
And some moments to breathe and grow in a direction other than family and community medicine. As a person, workmate, sister, daughter, artist, writer, et cetera.

.

With three generations of UPMDC alumni, and also three generations of doctors —Maryan, who requires no explanation; Raffy, now a clinical clerk enjoying (?) the practical application of medicine in PGH; RR, an IDS specialist now practicing somewhere in the bougie side of the world; and myself, still alive and smiling sometimes.
.
[I’ve made a lot of promises in the last few weeks about going out with friends and people… and then later not pushing through with it. It’s not you, it’s me. I’m just overwhelmed like that.]

This is me with Ate Risa during her birthday celebration last May. Or belated celebration. We watched a movie, ate good food, and also checked out Kindred PH, a wellness clinic in BGC that I really will try to write about at some point.
Life is mostly great.
.

.
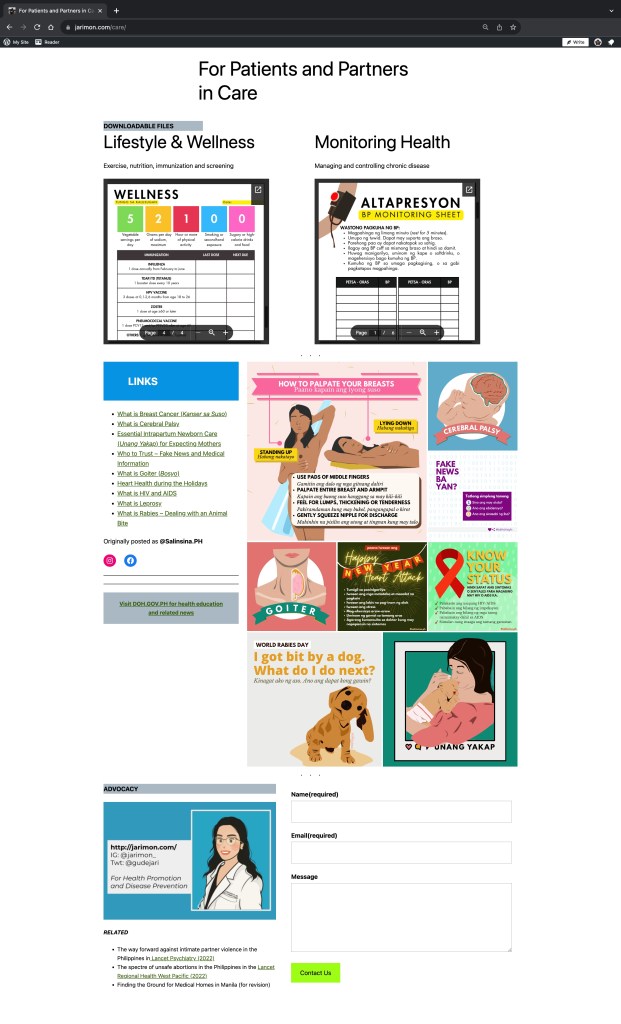
I also added a new passion-related page, featuring the cutest portrait art by Instagram commission artist @artsofae
.
Visit my new page: For Patients and Partners in Care
I’m still thinking if it’s worth making a Facebook or other social media page mirroring this blog. As this is mostly a personal log of all my thoughts and memories, and not really meant to build a brand or reputation… Ah, I don’t know.

.
Read more: Davao City 2023 – Life is Here
And a special thank you to the people who feed me, including but not limited to my gracious patients.

I’m actually writing this on what feels like an urgent internal deadline. Come tomorrow, I’ll be stuck in the Emergency Room from 7AM to 7PM everyday from Monday to Friday.
I hope to still have time to edit my research paper before its deadline, read some ECG tracings, go to ManilART, enjoy our batch teambuilding, and maybe read a book or two.
Actually I just hope to show up and survive. Here’s to the next fifteen months.
Until next time! ❤️

Say something back.