Every March I am reminded of my dad in two ways. First, we celebrate his birthday every 20th. Second, it happens to be Colon Cancer Awareness Month. It’s a tieback to the condition which eventually took my dad just shy of 38 years old. It’s also a regular reminder to take cancer prevention and early detection seriously, even at a young age.
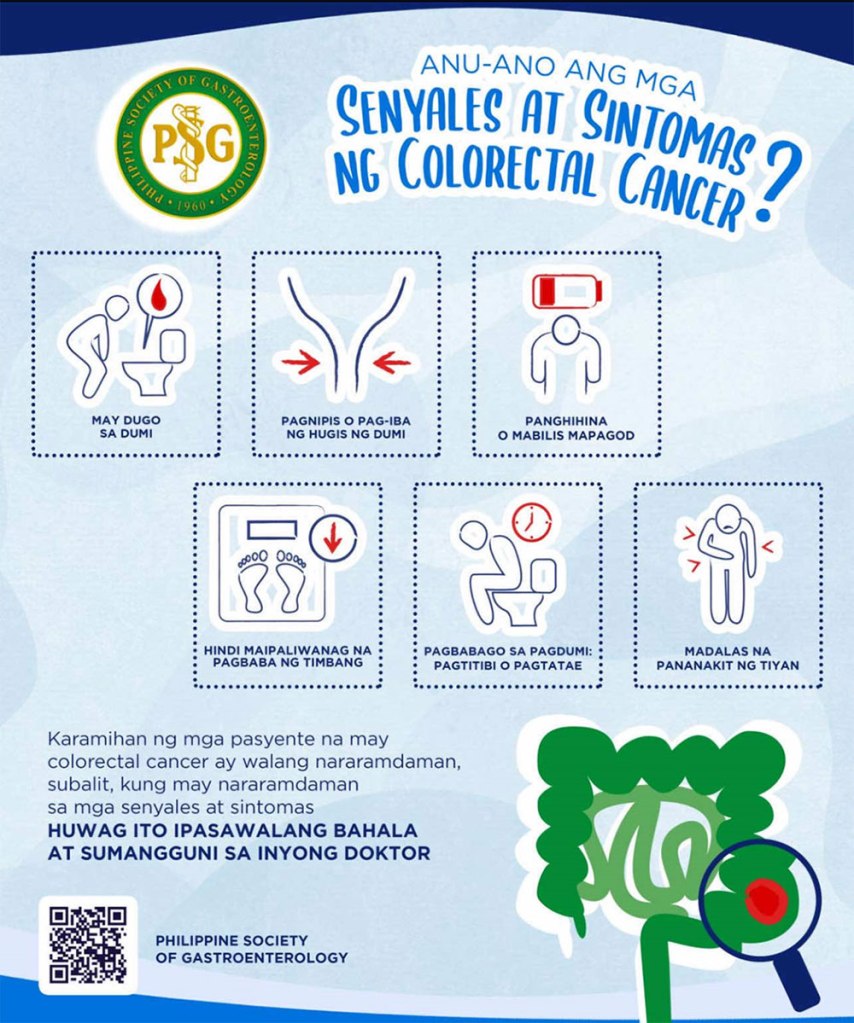
Colorectal cancer (colon cancer, cancer of the intestines, bukol sa bituka) is the third most common cancer in the Philippines. It’s also consistently among the top five cancer-related causes of death.

.
Early Detection Through Colon Cancer Screening
Now that I’m about to enter my 30s, it gets stranger and stranger to think that my dad died so young. He was even younger than Chadwick Boseman when he died. Not only does it feel strange, it also inspires some anxiety.
Anxiety is generally useless without action. That’s why I committed to finally getting myself screened for cancer. Screening means getting tested even if you don’t have symptoms. I prayed for negative results. But even if it turned out positive —which would be devastating, not gonna lie— earlier diagnosis still means better outcomes. At its early stages, colon cancer can be treatable. That’s true for most diseases.
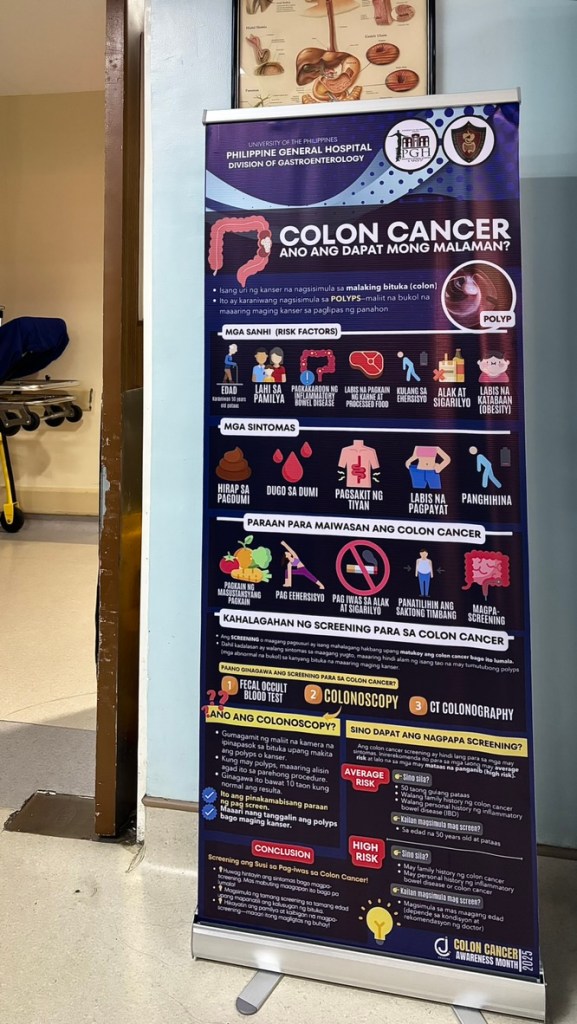
Screening for colon cancer can be done through colonoscopy, which is ideal but more invasive.
Screening for Colorectal Cancer
Not everyone has to be screened for colorectal cancer (CRC). Local guidelines recommend CRC screening starting at age 50. It is also recommended for those with:
- Personal history of colorectal cancer or advanced polyps
- Family history of cancer in the colon and rectum
- Certain diseases, like Inflammatory Bowel Disease
For people like me and my siblings, and especially older persons, I advocate for colonoscopy whenever available. Colonoscopy is an outpatient procedure where a small camera is directed carefully inside your body to visualize your intestinal walls. Most doctors would then recommend a repeat colonoscopy every 5 to 10 years.
Unfortunately, the procedure is not as common as the fecal tests. Colonoscopy can cost anywhere from PHP 15,000 to PHP 30,000, depending on the location, complications, and professional fees. It is covered by PhilHealth for all as inpatient service, and for select cases (Z benefit package) as outpatient.
There are also less invasive stool tests, which are recommended annually for the general population.
I got a colonoscopy for free at our national hospital.
My Experience: Free Colonoscopy at PGH
Colon Cancer Awareness Month is celebrated in the national hospital every year with a colonoscopy drive. There are increased slots for outpatient screening colonoscopies, including Saturday mornings. The procedure comes entirely free for general service patients, who will be attended to by fellows in training. It is offered at 40-50% off for patients willing to pay out-of-pocket for a specific consultant.
I decided to go as a general service patient to understand what it means when I navigate my patients to the unit. It was like going incognito, and a little surprise to the fellow-in-charge afterwards hahaha. (Also because the schedule seemed to fit best with my work, without having to go back-and-forth with a private consult.)
The process is easy and completely free aside, aside from time and travel well spent. It took around 3 weeks from start to end.
- Schedule your colonoscopy at the 3rd floor unit, main building.
- At least one week before the schedule: have the request approved at the outpatient PhilHealth office. This might take two working days if you’re employed, as your employer needs to sign on the papers.
- Two days before the colonoscopy: switch to a low-fiber diet (no meat and no vegetables).
- One day before the procedure: switch to a soft diet, then a clear liquid diet in the afternoon.
- Afternoon before the procedure: the most uncomfortable part, aka bowel prep with laxatives. For general service patients, this means taking an ungodly concoction of Bisacodyl and Castor Oil twice, all while hydrating with clear liquids. I absolutely HATE castor oil. Disgusting. Will not repeat if it can be helped ever again!!! The only saving grace was Pocari sweat and my juice drinks.
- Morning of the colonoscopy: Queue patiently (as with everything, it was first-come, first-serve).
- 6AM: Arrived to find I was 11th in line. 7AM: Waited to be called. Given papers to fill out. Changed into some pants. 9AM: Started procedure. 9:30AM: Ended procedure. 10AM: Discharged from clinic.
- I was able to catch up with our morning counseling lecture-workshop right after. I did feel a little bloated and tired from a night without sleep.
- Submit papers (the Claim Signature Form, or CSF) back to the PhilHealth Office. Claim results from colonoscopy unit.
I’m chagrined (???) to say I’ve apparently been misleading the patients that I previously referred to the Gastroenterology service for colonoscopy. I was under the impression that all colonoscopy procedures come with deep sedation. My only practical know-how comes from family’s experiences, which are closer to the pay or private experience than general services.
I had a colonoscopy under conscious sedation. I was awake the whole time, but almost 100% comfortable. I was put on low flow oxygen with monitor, a little BP cuff that never inflated, and some midazolam cocktail. Keeping me awake had the added benefit of getting to see my appendix and lonely diverticulum on the little TV. Cute.
In all, the experience was positive, mainly because I didn’t have any friable masses or suspicious polyps for biopsy. This blog would be so different if there were. The health care team were professional and relaxed.
I absolutely recommend having screening colonoscopy done if you have any of the risk factors. Take advantage of the colonoscopy drive that comes around once a year. On regular days, the waiting time for a screening colonoscopy is anywhere from 4 to 6 months.
Prevention is Still Better than Cure
We don’t really have a strong family history of CRC outside of my dad. My dad was well known for being incredibly smart, creative, and technologically savvy. But he was also a workaholic, chronic cigarette smoker, and daily alcoholic beverage drinker. I can say all these boldly because my dad is too comfortable in heaven to do anything about it.
Prevention is still better than cure. Lifestyle is key.
March is also a reminder and a challenge to:
- Stop or do not start cigarette smoking
- Avoid excessive alcohol consumption
- Modify obesity
- Avoid lack of exercise
- Avoid a diet that has high saturated fat, low fiber, and high red meat consumption
The good news (in general) is we’re living longer. The flip side? We have more time to experience mutations and lifestyle factors that contribute to cancer. This shift makes taking care of our health, and our family’s health, a top priority. Being proactive about prevention and early detection has moved from important to absolutely vital. I hope this moved the needle a little bit for you.
Until next time! ♥
Say something back.